Jackie's Take: What's on My Mind in Women's Wellness ✍ 🤔 📰
🧠 Mood, Midlife & the Truth About Hormone Therapy
You know the feeling. You’re in the middle of a meeting—or folding laundry, or walking the dog—and it hits you: Who am I right now?
You’re not exactly sad. Not exactly anxious. But definitely not yourself. Something between checked out, a little angry and emotionally underwater. A fog you can’t quite name.
It’s not dramatic enough to call depression, not disruptive enough to ring the alarm bells. But it’s there. Persistent. Flattening. Stealing your spark, your edge, your color.
And here's the hard part: If you try to explain this to your doctor, you're likely to hear one of two things:
“It’s probably stress—midlife is busy.”
“Your labs look normal.”
But let me be clear: normal doesn’t mean optimal, and this fog has a name. It’s hormonal. It’s neuroendocrine. It’s real. And it affects millions of women—especially during the perimenopause transition.
🔄 Mood & Midlife: A Hormonal Collision Zone
Perimenopause isn’t just hot flashes and weight gain. It’s a neurohormonal roller coaster, and mood is often the first cart off the rails.
📊 Studies confirm it:
According to the Study of Women’s Health Across the Nation (SWAN), women with a prior history of depression are up to twice as likely to experience depressive symptoms in perimenopause.
Reports have shown that up to 38% of women in perimenopause experience symptoms of depression.
A 2018 review found that menopause itself is an independent risk factor for major depression.
This is due in part to how estrogen interacts with serotonin, our feel-good neurotransmitter, and how declining progesterone affects GABA, the calming chemical that helps us sleep and self-regulate. When these hormones fluctuate or decline, the result can look like anxiety, sadness, or emotional burnout.
And let’s not forget: sleep disruption, brain fog, weight gain, fatigue, and sexual changes often layer on top of mood symptoms, making diagnosis—and relief—murkier.
💊 What Can Help? Cue the Hormone Therapy Conversation.
For years, hormone therapy was wrongly villainized. But we now know better.
The 2022 NAMS Position Statement confirms that hormone therapy (MHT), when started in the appropriate window (within 10 years of menopause), is safe for most healthy women and offers multiple benefits, including:
✅ Improved sleep
✅ Reduced hot flashes and night sweats
✅ Better bone health
✅ Improved mood and sense of well-being
In fact, estrogen may enhance the effects of antidepressants for women with treatment-resistant depression in midlife. And for women who had their ovaries removed prematurely, MHT can help prevent severe and prolonged mood disruption due to abrupt hormonal loss.
And no, it’s not just estrogen. Progesterone plays a crucial role, too—particularly in calming anxiety and promoting sleep. The right combination, dosing, and delivery method of MHT is part art, part science, and highly individual.
🏛️ So Why Aren’t More Women Offered This?
Because we’re still undoing decades of misinformation.
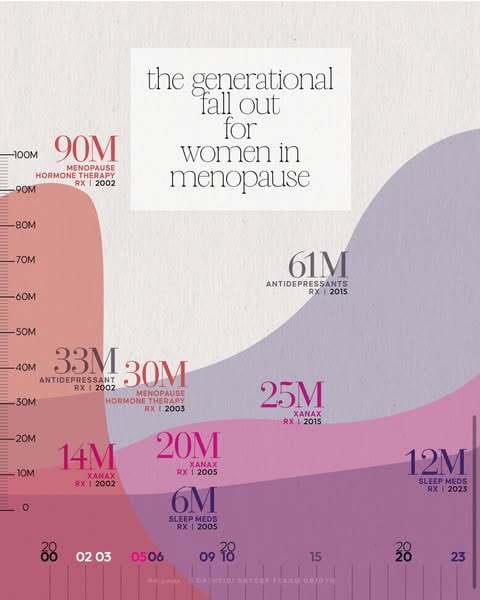
The 2002 WHI study that scared an entire generation off MHT has since walked back many of its original conclusions. Most notably, estrogen-only therapy was shown to reduce the risk of breast cancer and all-cause mortality in long-term follow-up. But the damage was done. Millions of women were taken off their hormones overnight—and many still haven’t been offered a way back.
In the aftermath, we saw something else spike: prescriptions for Xanax, SSRIs, and sleep medications (see the brilliant illustration below via Dr Heidi Flagg). Instead of addressing the hormonal shifts, women were increasingly medicated for the symptoms—mood swings, anxiety, insomnia—that hormone therapy had previously been helping to stabilize. The result? A generation of women sedated and sidelined, rather than supported.
That’s finally starting to shift.
Just this past week, a landmark FDA hearing gathered top menopause experts—including my colleagues and mentors—who urged the agency to modernize its guidance and finally approve testosterone for women, while also updating the outdated “black box” warnings on hormone therapy (FDA panel summary here).
One of the points raised? That emerging evidence supports the use of transdermal testosterone for more than just sexual functioning in women. A 2024 retrospective UK cohort study showed that four months of testosterone therapy significantly improved mood and cognition in menopausal women. While not FDA-approved for this indication yet, the clinical tide is shifting.
💬 So What Should You Do?
But before that, I want you to know—it’s not just you. I’ve been feeling it too.
Maybe it’s stress (I’ve been working hard on something I can’t wait to share with you this Fall). Maybe it’s the kids—mine are in and out of camps and sleepaway, and I miss them. Maybe it’s the heat. Maybe it’s the lack of routine. Or maybe… it’s that I’m 45, and this is just what shifting feels like.
So here’s what I’ve tried this week:
☀️ After-dinner walks to get sundown light in my eyes (circadian rhythm syncing).
🍪 Baking. (I don’t even particularly like to bake—but something sweet and new felt right.)
🛍 A little shopping for an upcoming speaking event—because sometimes a new outfit gives you just the right amount of dopamine.
💉 And this morning? A pump of testosterone—because it felt like I needed it.
None of these things are magic. But they’re signals. Data points. Invitations to tune in more closely.
So if you feel off—not yourself, not broken, but not quite right—don’t dismiss it.
Instead, ask:
Could this be related to perimenopause?
Would a trial of hormone therapy make sense for me?
How can I better understand the connection between my hormones and my mood?
Midlife mood changes aren’t just inconvenient—they’re instructive.
You don’t need to power through, numb out, or wait until it gets worse.
You need—and deserve—a care plan that actually sees you and evolves with you.
Let this be your nudge to ask more, expect more, and start the conversation.
💬 Let’s Keep the Conversation Going
Hey there! Quick favor before you scroll—TAP THE ANSWER in the poll below that fits you best (and drop me a comment, I really love hearing from you)🙏 ⤵
Tell me which is your MOST challenging peri symptom right now?
The Tea: What's Trending in Women's Wellness & Culture 🍵 🛍
The best workout might not be the one that burns the most, but rather the one that actually fits your personality. Introverts, extroverts, Type A planners, chaos lovers—your movement sweet spot might be more psychological than physical.
Personally, I’ve been playing around with Enneagram stuff lately (not for sport—I'm building something 👀), and honestly? It tracks. I’m realizing I need workouts that make me feel competent and in control, but not bored to death. 🎽(Time)
A new global metabolic study basically upends everything we were told in the early 2000s: inactivity is not the main cause of obesity. Turns out, people in industrialized countries burn about the same number of calories as hunter-gatherers. The problem? We’re eating more—and mostly ultra-processed junk. 🧬💥 (WaPo)
I’m loving this recap of the standout moments from this year’s New York Times Well Festival. It’s giving smart, evidence-backed, and refreshingly non-cringe. Highlights include: stress is more toxic than sugar (yes), weight loss drugs aren’t magic (also yes), and social connection still reigns supreme for healthspan.
I love when wellness gets this real. It’s not about biohacks—it’s about nervous system regulation, good boundaries, and people who text you back. Less hustle, more homeostasis (easier said than done, but I’m trying). 7⃣🔎 (SuperAge)
♋ 💉Research Corner: GLP-1 Receptor Agonists Show Promise as Adjunctive Treatment for Ovarian Cancer
According to AJMC, early research suggests GLP-1 receptor agonists—yes, the Ozempic class—may hold promise as an adjunctive treatment for ovarian cancer. While still in the early stages, the proposed mechanisms include anti-inflammatory and anti-proliferative effects, along with improved insulin sensitivity.
Personally, I’d love to see a study looking at breast cancer risk or even breast density changes in women using GLPs. We know breast density is linked to inflammation—and both are connected to cancer risk. 🤔
The Group Chat Edit 📲 👯♂
🔉To Listen: SJP on Las Culturistas 👠
Wherever Carrie Bradshaw goes, I will faithfully follow. Matt & Bowen talk to SJP about the evolution of her shoe game and much more. 🎙
🛍 To Buy: A Cheese Subscription That Ages Beautifully🧀
If you haven’t browsed Murray’s Cheese Clubs, you’re missing out on peak gift energy—from NYC’s most iconic cheese shop. Choose from 3, 6, or 12-month subscriptions and take their “Find Your Main Cheese” quiz while you’re at it. It’s the personality test you never knew you needed.👩🍳
😀To Try: How to Fold a Towel Like the Four Seasons 🏩
It’s the little things, my friends. 🏖
Saddle Up & Spread the Word 🏇💨

If you’re still reading, thank you. In the early days of a business, every subscribe, like, and share makes a real difference. Your early support means so much as I keep building In the Saddle - both the newsletter and this community ⭕
To share — Just click and copy this link: https://inthesaddle.beehiiv.com/
If you’re a brand, expert, or just someone with an excellent story to tell in the wellness, longevity, or sexual health space, I’d love to connect! I am always open to hearing ideas for ITS content and collabs. ✏️ 🏇🔥
With gratitude always,
Jackie Giannelli, FNP-BC, MSCP
Founder, In the Saddle
What did you think of today's newsletter?
Medical Disclaimer:
The content provided in this newsletter is for informational and educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Nothing contained herein should be construed as medical guidance or the practice of medicine. You should always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay seeking care because of something you read in this newsletter. Use of the information provided is at your own risk. No clinician-patient relationship is formed through this content.